Jaundice, a condition characterized by the yellowing of the skin and eyes, is a result of elevated levels of bilirubin in the bloodstream. Understanding its symptoms, underlying causes, and appropriate treatment options is crucial for effective management. Let’s delve into the multifaceted aspects of jaundice to comprehend its nuances and tackle this condition effectively.
Pages of Contents
I. Introduction to Jaundice
Definition and Overview
Jaundice, medically known as icterus, manifests as a yellow discoloration of the skin, mucous membranes, and sclera due to increased bilirubin levels. Bilirubin, a byproduct of red blood cell breakdown, is typically processed by the liver and excreted in bile.
Causes of Jaundice
Various factors contribute to jaundice, including liver diseases like hepatitis, cirrhosis, and liver cancer, as well as hemolytic disorders, such as sickle cell anemia or thalassemia. Additionally, bile duct obstruction, Gilbert’s syndrome, and certain medications can induce jaundice.
II. Understanding Jaundice Symptoms
Yellowing of the Skin and Eyes
One of the primary and most visible symptoms of jaundice is the yellowing of the skin and whites of the eyes, indicating an excess of bilirubin in the bloodstream.
Other Visible Signs
Apart from skin discoloration, individuals might experience dark-colored urine, pale stools, and itching due to jaundice.
Associated Symptoms
Accompanying symptoms might include fatigue, abdominal pain, nausea, vomiting, and loss of appetite, depending on the underlying cause.
III. Diagnostic Methods for Jaundice
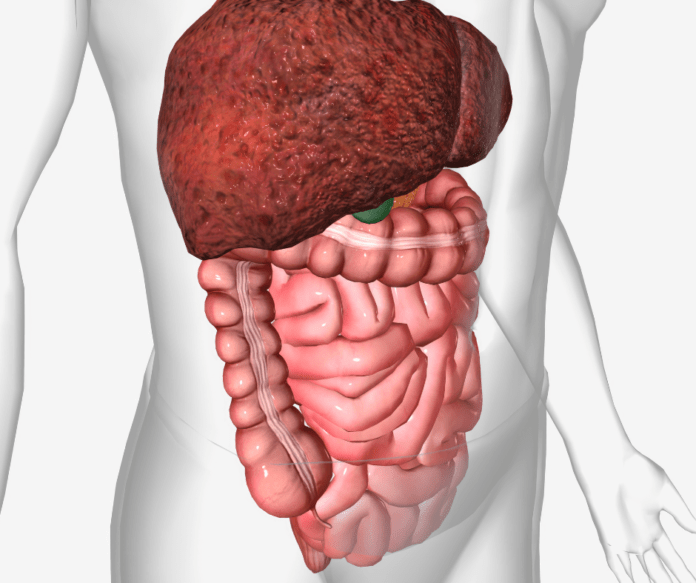
Physical Examination
Healthcare providers conduct a thorough physical examination, checking for yellowing of the skin, abdominal tenderness, and enlargement of the liver or spleen.
Blood Tests for Bilirubin Levels
Blood tests measuring total and direct bilirubin levels help in diagnosing the severity and type of jaundice.
Imaging Techniques
Imaging studies like ultrasound, CT scans, or MRIs assist in identifying potential causes such as gallstones, tumors, or liver abnormalities.
IV. Types of Jaundice
Pre-Hepatic Jaundice
This type results from increased breakdown of red blood cells, leading to excess bilirubin production, often caused by conditions like hemolytic anemia.
Hepatic Jaundice
Hepatic jaundice stems from liver diseases that impair bilirubin processing, such as hepatitis or cirrhosis.
Post-Hepatic Jaundice
Obstruction of bile flow, commonly due to gallstones or tumors, causes post-hepatic jaundice, hindering bilirubin excretion.
V. Complications Related to Jaundice
Liver Damage
Untreated jaundice can lead to progressive liver damage, potentially culminating in liver failure.
Gallstones
Obstruction of bile flow increases the risk of developing painful gallstones, further exacerbating the condition.
Encephalopathy
In severe cases, the accumulation of toxins due to impaired liver function can lead to encephalopathy, causing confusion and altered mental status.
VI. Treatment Options for Jaundice
Addressing Underlying Causes
Treating the underlying condition, whether liver disease, hemolysis, or obstruction, forms the crux of jaundice management.
Medications and Therapies
Depending on the cause, medications to increase bile flow, blood transfusions, or therapies to improve liver function might be prescribed.
Surgical Interventions
Surgery might be necessary to remove obstructions, like gallstones or tumors, to alleviate bile flow blockages.
VII. Lifestyle and Home Remedies
Diet Modifications
Adopting a low-fat, high-fiber diet can aid liver function and help manage jaundice.
Hydration
Adequate hydration supports overall liver health and aids in bile production and excretion.
Avoiding Alcohol and Toxins
Eliminating alcohol consumption and avoiding exposure to toxins helps reduce further liver damage.
VIII. Prevention Strategies
Vaccinations
Vaccinations against hepatitis A and B can prevent certain liver infections that might lead to jaundice.
Healthy Lifestyle Practices
Maintaining a healthy weight, exercising regularly, and avoiding risky behaviors reduce the risk of liver diseases.
Regular Medical Check-ups
Periodic health check-ups enable early detection and management of conditions that might lead to jaundice.
IX. Jaundice in Specific Demographics
Newborns and Jaundice
Newborns often experience physiological jaundice, which typically resolves without treatment; however, severe cases might necessitate medical intervention.
Jaundice in Adults
Adults experiencing jaundice should promptly seek medical attention to diagnose and treat the underlying cause.
Elderly and Jaundice
Elderly individuals with jaundice might have complex health issues requiring specialized care and management.
X. Conclusion
In conclusion, jaundice, though symptomatic in its yellowing manifestation, stems from various underlying causes. Early diagnosis through careful examination, understanding its types, and timely intervention can significantly impact effective management. Addressing lifestyle, treating the root cause, and preventive measures are crucial for mitigating the complications associated with jaundice. Understanding the nuances of this condition empowers individuals to seek timely medical attention, ensuring better outcomes and overall liver health.